-
Home
-
About JCTR
-
Gold Open Access
-
Issues
-
Editorial board
-
Author guidelines
-
Publication fees
-
Online first
-
Special issues
-
News
-
Publication ethics
-
Partners
-
Submit your manuscript
-
Submit your review report
-
Editorial Office
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. ISSN print: 2382-6533 ISSN online: 2424-810X
Volume 1 Issue 1
Laser-assisted vascular welding: optimization of acute and post-hydration welding strength
Dara R. Pabittei, Michal Heger, Marc Simonet, Sjoerd van Tuijl, Allard C. van der Wal, Ed van Bavel, Ron Balm, Bas A. de Mol
Pabittei et al., J Clin Transl Res, 2015; 1(1) : 31-47
Published online: 21 June, 2015
Abstract
Background: Liquid solder laser-assisted vascular welding using biocompatible polymeric scaffolds (ssLAVW) is a novel technique for vascular anastomoses. Although ssLAVW has pronounced advantages over conventional suturing, drawbacks include low welding strength and extensive thermal damage.
Aim: To determine optimal ssLAVW parameters for maximum welding strength and minimal thermal damage.
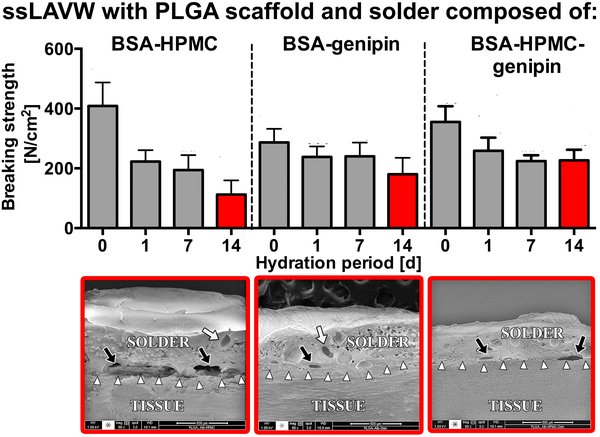
Methods: Substudy 1 compared breaking strength (BS) of aortic strips welded with electrospun poly(ε-caprolactone) (PCL) or poly(lactic-co-glycolic acid) (PLGA) scaffold, 670-nm laser, 50-s single-spot continuous lasing (SSCL), and semi-solid solder (48% bovine serum albumin (BSA)/0.5% methylene blue (MB)/3% hydroxypropylmethylcellulose (HPMC)). Substudy 2 compared the semi-solid solder to 48% BSA/0.5% MB/0.38% genipin and 48% BSA/0.5% MB/3% HPMC/0.38% genipin solder. Substudy 3 compared SSCL to single-spot pulsed lasing (SSPL).
Results: PCL-ssLAVW yielded an acute BS of 248.0±54.0N/cm2 and remained stable up to 7d of hydration. PLGA-ssLAVW obtained higher acute BS (408.6±78.8N/cm2) but revealed structural defects and a BS of 109.4±42.6N/cm2 after14d of hydration. The addition of HPMC and genipin improved the 14-d BS of PLGA-ssLAVW (223.9±19.1N/cm2). Thermal damage was reduced with SSPL compared with SSCL.
Conclusions: PCL-ssLAVW yielded lower but more stable welds than PLGA-ssLAVW. The addition of HPMC and genipin to the solder increased the post-hydration BS of PLGA-ssLAVW. SSPL regimen reduced thermal damage. PLGA-ssLAVW using 48% BSA/0.5% MB/3% HPMC/0.38% genipin solder and SSPL constitutes the most optimal welding modality.
Relevance for patients: Surgical patients requiring vascular anastomoses may benefit from the advantages that ssLAVW potentially offers over conventional (gold standard) sutures. These include no needle trauma and remnant suture materials in the patient, reduction of foreign body reaction, immediate liquid-tight sealing, and the possibility of a faster and easier procedure for minimally invasive and endoscopic anastomotic techniques.
DOI: http://dx.doi.org/10.18053/jctres.201501.001
Author affiliation
1 Department of Cardio-thoracic Surgery, Academic Medical Center, University of Amsterdam, Meibergdreef 9, 1105 AZ Amsterdam, the Netherlands;
2 Department of Surgery, Academic Medical Center, University of Amsterdam, Meibergdreef 9, 1105 AZ Amsterdam, the Netherlands;
3 Department of Experimental Surgery, Academic Medical Center, University of Amsterdam, Meibergdreef 9, 1105 AZ Amsterdam, the Netherlands;
4 Department of Biomedical Engineering, Material Technology, Technical University Eindhoven, PO Box 513, 5600 MB Eindhoven, the Netherlands;
5 HemoLab, Den Dolech 2, 5612 AZ Eindhoven, the Netherlands;
6 Department of Pathology, Academic Medical Center, University of Amsterdam, Meibergdreef 9, 1105 AZ Amsterdam, the Netherlands;
7 Department of Biomedical Engineering and Physics, Academic Medical Center, University of Amsterdam, Meibergdreef 9, 1105 AZ Amsterdam, the Netherlands.
*Corresponding author:
Michal Heger
Department of Experimental Surgery, Academic Medical Center
Meibergdreef 9, 1105 AZ Amsterdam, the Netherlands
Tel: +31 20 5665573
E-mail: m.heger@amc.uva.nl
Handling editor:
Bernard Choi
Beckman Laser Institute and Medical Clinic, University of California, Irvine, CA, United States
Department of Biomedical Engineering, University of California, Irvine, CA, United States
Downloads
Peer review process file (331.7 KB)
Supplemental figure 1 (20.4 MB)
Supplemental figure 2 (25.0 MB)

