-
Home
-
About JCTR
-
Gold Open Access
-
Issues
-
Editorial board
-
Author guidelines
-
Publication fees
-
Online first
-
Special issues
-
News
-
Publication ethics
-
Partners
-
Submit your manuscript
-
Submit your review report
-
Editorial Office
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. ISSN print: 2382-6533 ISSN online: 2424-810X
Volume 9 Issue 3
Therapeutic outcomes of early and delayed ERCP and PTCD in patients with obstructive severe acute biliary pancreatitis
Xue Ling Zhang†, Jia Huan Sun†, Yue Wu, Min Xie, Cong Cong Li, Dong Lv, Wei Yu*, Pei Lin Cui*
Zhang et al. J Clin Transl Res 2023; 9(3):7
Published online: May 15, 2023
Abstract
Background: Obstructive severe acute biliary pancreatitis (SABP) is a clinical emergency with a high rate of mortality that can be alleviated by endoscopic retrograde cholangiopancreatography (ERCP) and percutaneous transhepatic cholangial drainage (PTCD) selectively. However, the optimal timing of ERCP and PTCD requires elucidation.
Aim: To evaluate outcome parameters in patients with SABP subjected to ERCP and PTCD compared to SABP patients who were not subjected to any form of invasive intervention.
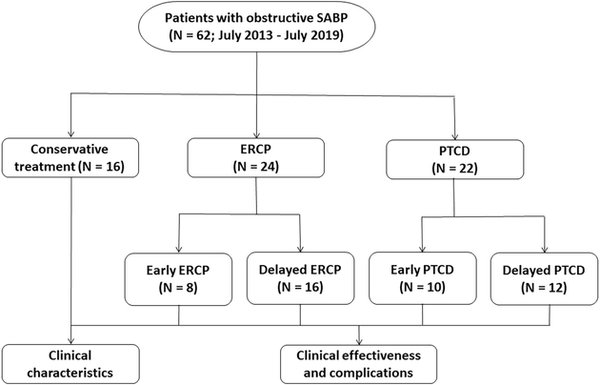
Methods: A total of 62 patients with obstructive SABP who had been treated from July 2013 to July 2019 were included in this retrospective case-control study and stratified into a PTCD group (N = 22), ERCP group (N = 24), and conservative treatment group (N = 16, control). Patients in the PTCD and ERCP groups were substratified into early (≤ 72 h) and delayed (> 72 h) treatment groups based on the timing of the intervention after diagnosis. Clinical chemistry, hospitalization days, liver function, abdominal pain, and complications were determined to assess treatment efficacy and safety of each modality and to establish the optimal timing for PTCD and ERCP.
Results: The average hospitalization time, time to abdominal pain relief, and time to normalization of hematological and clinical chemistry parameters (leukocyte count, amylase, ALT, and total bilirubin) were shorter in the PTCD and ERCP group compared to the conservative treatment group (p < 0.05). The average hospitalization time in the ERCP group (16.7 ± 4.0 d) was shorter compared to the PTCD group (19.6 ± 4.3 d) (p < 0.05). Compared to the conservative treatment group (62.5%), there were more complications in patients treated with ERCP and PTCD (p < 0.05). In the early ERCP group, the average hospitalization time (13.9 ± 3.3 d) and the time to normalization of leukocyte count (6.3 ± 0.9 d) and total bilirubin (9.1 ± 2.0 d) were lower than in the delayed ERCP group (18.6 ± 4.1 d, 9.9 ± 2.4 d, 11.8 ± 2.9 d, respectively) and early PTCD group (16.4 ± 3.7 d, 8.5 ± 2.1 d, 10.9 ± 3.1 d, respectively) (p < 0.05). In the delayed ERCP group, the average hospitalization time (18.6 ± 4.1 d) and ALT recovery time (12.2 ± 2.6 d) were lower than in the delayed PTCD group (21.9 ± 4.3 d and 14.9 ± 3.9 d, respectively) (p < 0.05).
Conclusions: ERCP and PTCD effectively relieve SABP-associated biliary obstruction with comparable overall incidence of complications. It is recommended that ERCP is performed within 72 h after diagnosis; and PTCD drainage may be considered as an alternative approach in cases where patients are unable or unwilling to undergo ERCP or ERCP is unsuccessful.
Relevance for patients: ERCP and PTCD in patients with obstructive SABP can resolve biliary obstruction and delay progression of the disease. Performing ERCP and PTCD within 72 h (i.e., optimal treatment time window) can be beneficial to patients, especially in terms of post-operative recovery. Visual biliary endoscopy (oral or percutaneous transhepatic) may be used for concomitant therapeutic interventions in the biliary system.
†These authors contributed equally to this work
DOI: http://dx.doi.org/10.18053/jctres.09.202303.007
Author affiliation
1. Department of International Medical Services (IMS), Beijing Tiantan Hospital, Capital Medical University
2. Department of Gastroenterology, Beijing Tiantan Hospital, Capital Medical University
3. Department of General Surgery, Beijing Tiantan Hospital, Capital Medical University
*Corresponding author
Wei Yu
Department of General Surgery, Beijing Tiantan Hospital, Capital Medical University, Beijing 100070, China.
Email: yuweimade@sina.com
Handling editor:
Michal Heger
Department of Pharmaceutics, Utrecht University, the Netherlands
Department of Chemistry, Utrecht University, Utrecht, the Netherlands
Department of Pathology, Erasmus Medical Center, the Netherlands
Department of Pharmaceutics, Jiaxing University Medical College, Zhejiang, China

