-
Home
-
About JCTR
-
Gold Open Access
-
Issues
-
Editorial board
-
Author guidelines
-
Publication fees
-
Online first
-
Special issues
-
News
-
Publication ethics
-
Partners
-
Submit your manuscript
-
Submit your review report
-
Editorial Office
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. ISSN print: 2382-6533 ISSN online: 2424-810X
Volume 9 Issue 3
Trends in place of death in patients with idiopathic pulmonary fibrosis: a ten-year analysis of the United States National Center for Health Statistics WONDER database
Yousaf Hadi, Amir Humza Sohail, Emily Schiller*, Meher Oberoi, Syeda Naqvi, Muhammad Aziz, Hira Rohail, Ali Khan; Muhammad Salman Khan, Collin E.M. Brathwaite, Micheal Khalife, Sarah Hadique
Hadi et al. J Clin Transl Res 2023; 9(3):2
Published online: April 15, 2023
Abstract
Background: Idiopathic pulmonary fibrosis (IPF) has a poor prognosis and carries a high mortality rate. For patients with advanced IPF, death at home or in hospice may be associated with improved quality of life, but data regarding place of death in IPF is lacking.
Aim: To study temporal trends in the place of death for patients dying with IPF.
Methods: We utilized a publicly reported platform to study the place of death in patients with IPF. The United States National Center for Health Statistics (NCHS) WONDER platform was used to access mortality data based on death certificates of all mortalities in the United States for the years 2008-2017. All patients with IPF as the underlying cause of death were included. Mann-Kendall trend test was applied to identify temporal trends.
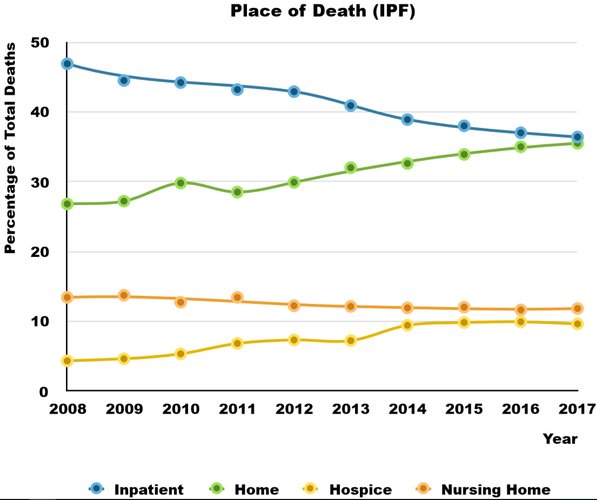
Results: There were a total of 133200 deaths with IPF as the underlying diagnosis during the study period, with a crude rate of 4.2 per 100,000 deaths. 41%, 21%, 7.5% and 12.5% of deaths occurred in inpatient facilities, at home, in hospice, and in nursing homes/long term care facilities, respectively.
The percentage of deaths in hospice facilities significantly increased during the study period (4.3% in 2008 to 9.6% in 2017; p value < 0.001). This was accompanied by an increase in deaths at home from 26.8% in 2008 to 35.5% in 2017 (p value <0.01) and a decrease in inpatient deaths from 46.9% in 2008 to 36.4% in 2017 (p value <0.01).
A greater proportion of females died in hospice compared to males (7.81% vs 7.27%, p value < 0.0001). Compared to all other race groups, white patients more frequently died in hospice (7.77% vs 4.67%, p value <0.001).
Conclusions: Hospice is underutilized in IPF patients. There is disparity in the use of hospice both in gender and ethnicity, although the disparity in gender may not be clinically relevant.
Relevance for patients: Given the high morbidity and mortality of IPF, early involvement of supportive care and palliation is essential to maximizing the quality of the end-of-life in this patient population
DOI: http://dx.doi.org/10.18053/jctres.09.202303.002
Author affiliation
1. Department of Medicine, West Virginia University, Morgantown, West Virginia, United States of America
2. Department of Surgery, NYU Langone Long Island Hospital, Mineola, New York, United States of America
3. NYU Long Island School of Medicine, Mineola, New York, United States of America
4. Department of Medicine, University of Toledo, Toledo, Ohio, United States of America
5. St. George’s University School of Medicine, St. George’s, Grenada
6. Department of Medicine, Trinity Health Oakland Hospital, Pontiac, Michigan, United States of America
7. Department of Diagnostic and Interventional Imaging , University of Texas Health Science Center, Houston, Texas, United States of America
*Corresponding author
Emily Schiller
NYU Long Island School of Medicine, Mineola, New York, United States of America
Email: Emily.Schiller@nyulangone.org
Handling editor:
Michal Heger
Department of Pharmaceutics, Utrecht University, the Netherlands
Department of Chemistry, Utrecht University, Utrecht, the Netherlands
Department of Pathology, Erasmus Medical Center, the Netherlands
Department of Pharmaceutics, Jiaxing University Medical College, Zhejiang, China

