-
Home
-
About JCTR
-
Gold Open Access
-
Issues
-
Editorial board
-
Author guidelines
-
Publication fees
-
Online first
-
Special issues
-
News
-
Publication ethics
-
Partners
-
Submit your manuscript
-
Submit your review report
-
Editorial Office
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. ISSN print: 2382-6533 ISSN online: 2424-810X
Volume 9 Issue 2
Acute acalculous cholecystitis as a rare gastroenterological association of COVID-19: a case series and systematic review
Junaid Rasul Awan, Zahra Akhtar, Faisal Inayat*, Aimen Farooq, Muhmmad Hassan Naeem Goraya, Rizwan Ishtiaq, Sana Malik, Fariha Younus, Sana Kazmi, Muhammad Junaid Ashraf, Ahmad Azeem Khan, Zahid Ijaz Tarar
Awan et al. J Clin Transl Res 2023; 9(2):10
Published online: March 28, 2023
Abstract
Background and aim: Acute acalculous cholecystitis (AAC) is an acute inflammatory disease of the gallbladder in the absence of cholecystolithiasis. It is a serious clinicopathologic entity, with a high mortality rate of 30%–50%. A number of etiologies have been identified that can potentially trigger AAC. However, clinical evidence on its occurrence following COVID-19 remains scarce. We aim to evaluate the association between COVID-19 and AAC.
Methods: We report our clinical experience based on 3 patients who were diagnosed with AAC secondary to COVID-19. A systematic review of the MEDLINE, Google Scholar, Scopus, and Embase databases was conducted for English-only studies. The latest search date was December 20, 2022. Specific search terms were used regarding AAC and COVID-19, with all associated permutations. Articles that fulfilled the inclusion criteria were screened, and 23 studies were selected for a quantitative analysis.
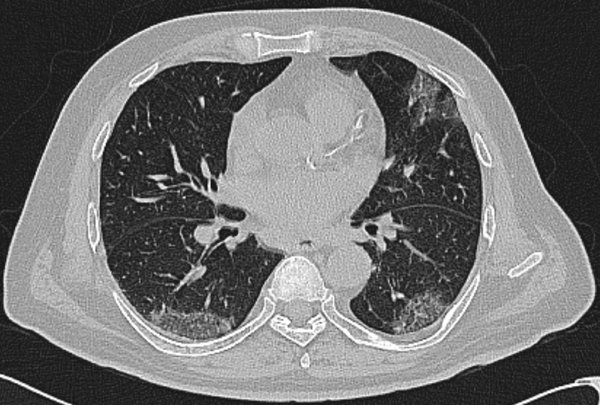
Results: A total of 31 case reports (level of clinical evidence: IV) of AAC related to COVID-19 were included. The mean age of patients was 64.7 ± 14.8 years, with a male-to-female ratio of 2.1:1. Major clinical presentations included fever 18 (58.0%), abdominal pain 16 (51.6%), and cough 6 (19.3%). Hypertension 17 (54.8%), diabetes mellitus 5 (16.1%), and cardiac disease 5 (16.1%) were among the common underlying medical conditions. In our analysis of initial presentation patterns, COVID-19 pneumonia was encountered before, after, or concurrently with AAC in 17 (54.8%), 10 (32.2%), and 4 (12.9%) patients, respectively. Coagulopathy was noted in 9 (29.0%) patients. Imaging studies for AAC included CT scan and ultrasonography in 21 (67.7%) and 8 (25.8%) cases, respectively. Based on the Tokyo Guidelines 2018 criteria for severity, 22 (70.9%) had grade II and 9 (29.0%) patients had grade I cholecystitis. Treatment included surgical intervention in 17 (54.8%), conservative management alone in 8 (25.8%), and percutaneous transhepatic gallbladder drainage in 6 (19.3%) patients. Clinical recovery was achieved in 29 (93.5%) patients. Gallbladder perforation was encountered as a sequela in 4 (12.9%) patients. The mortality rate in patients with AAC following COVID-19 was 6.5%.
Conclusions: We report AAC as an uncommon but important gastroenterological complication following COVID-19. Clinicians should remain vigilant for COVID-19 as a possible trigger of AAC. Early diagnosis and appropriate treatment can potentially save patients from morbidity and mortality.
Relevance for Patients: AAC can occur in association with COVID-19. If left undiagnosed, it may adversely impact the clinical course and outcomes of patients. Therefore, it should be considered among the differential diagnoses of right upper abdominal pain in these patients. Gangrenous cholecystitis can often be encountered in this setting, necessitating an aggressive treatment approach. Our results point out the clinical importance of raising awareness about this biliary complication of COVID-19, which will aid in early diagnosis and appropriate clinical management.
DOI: http://dx.doi.org/10.18053/jctres.09.202302.010
Author affiliation
1. University Hospital Limerick, Limerick, Ireland
2. University of Texas Medical Branch, Galveston, TX, USA
3. Allama Iqbal Medical College, Lahore, Pakistan
4. Advent Health Florida, Orlando, FL, USA
5. Saint Francis Hospital and Medical Center, Hartford, CT, USA
6. University Maternity Hospital Limerick, Limerick, Ireland
7. Dow University of Health Sciences, Karachi, Pakistan
8. University of Missouri School of Medicine, Columbia, MO, USA
*Corresponding author
Faisal Inayat
Allama Iqbal Medical College, Allama Shabbir Ahmad Usmani Road, Faisal Town, Lahore 54550, Punjab, Pakistan.
Tel: +92 321 774 3758
Fax: +92 42 9923 1443
Email: faisalinayat@hotmail.com
Handling editor:
Michal Heger
Department of Pharmaceutics, Utrecht University, the Netherlands
Department of Chemistry, Utrecht University, Utrecht, the Netherlands
Department of Pathology, Erasmus Medical Center, the Netherlands
Department of Pharmaceutics, Jiaxing University Medical College, Zhejiang, China

