-
Home
-
About JCTR
-
Gold Open Access
-
Issues
-
Editorial board
-
Author guidelines
-
Publication fees
-
Online first
-
Special issues
-
News
-
Publication ethics
-
Partners
-
Submit your manuscript
-
Submit your review report
-
Editorial Office
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. ISSN print: 2382-6533 ISSN online: 2424-810X
Volume 9 Issue 2
Spatiotemporal gait and fatigue do not change when using common at-home gait tasks in patients with Facioscapulohumeral Muscular Dystrophy: a pilot study
Nicholas G. Murray*, Marie Kelly, Vipul Lugade, Ryan Wuebbles, Madison Taylor, Douglas Powell, Takako Jones, Peter Jones
Murray et al. J Clin Transl Res 2023; 9(2):4
Published online: February, 7 2023
Abstract
Background: Facioscapulohumeral Dystrophy (FSHD) is the third most common muscular dystrophy, with para-spinal, trunk, and thigh muscles being affected earlier in the disease progression than previously believed. Gait declines are a possible marker of disease progression of FSHD, however, gait assessment typically requires patients to travel directly to a specific collection site. The introduction of smart-phone applications to measure gait may be a viable way of tracking longitudinal gait decline in FSHD. Yet it is not established which gait tasks are appropriate for this unique and varying population.
Aim: This paper investigates if three commonly used gait tasks in FSHD are appropriate for use in an at-home setting when collected using a smart-phone gait analyzer application.
Methods: Eight genetically confirmed FSHD individuals completed three gait tasks at-home using a custom made smart-phone gait analyzer application. These included the most common gait tasks reported in the FSHD literature 1) 12 consecutive walking trials over a ten-meter level surface, 2) 6 consecutive walking trials across a ten-meter level surface in the morning and afternoon (a minimum of 4 hours between testing) and 3) ambulating for as long as they can for 6-minutes. Two repeated measures ANCOVAs were used to examine velocity and cadence changes across the gait tasks while controlling for shoe type, surface, and the use of an assistive device. Three Wilcoxon Signed Ranks tests analyzed the delta self-reported fatigue score by each gait task.
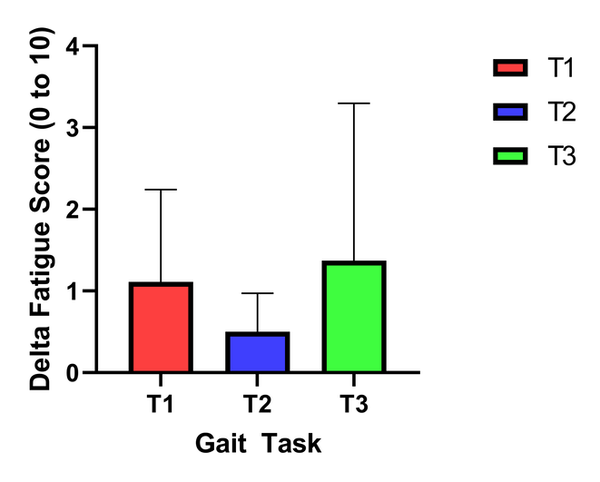
Results: No significant difference was noted between the three gait tasks for gait velocity and cadence. FSHD patients self-reported that the 6-minute walk test was the most difficult, however, the delta fatigue score was not different between the gait tasks but had a moderate effect size compared to the 12 meter conservative walking. This is most likely due to the small and heterogeneous sample size but indicates the 6-minute walk test may be more physically demanding.
Conclusion: Patients with FHSD can successfully complete varying at-home walking protocols without eliciting a great deal of fatigue or significant change in spatiotemporal gait.
Relevance to patients: These three gait protocols could be used interchangeably for the evaluation of gait in FSHD at-home using the valid and reliable Gait Analyzer application. This will decrease the travel requirements for patients to attend in-person gait evaluations for research and clinical studies.
DOI: http://dx.doi.org/10.18053/jctres.09.202302.004
Author affiliation
1. Neuromechanics Laboratory, School of Public Health, University Of Nevada, Reno, United States of America
2. Decker College of Nursing and Health Sciences, Division of Physical Therapy, Binghamton University, New York, NY, United States of America
3. University of Nevada, Reno School of Medicine, Department of Pharmacology, Reno, NV, United States of America
4. University of Memphis, College of Health Sciences, Memphis, TN, United States of America
*Corresponding Author:
Nicholas Murray
Neuromechanics Laboratory, School of Public Health, University Of Nevada, Reno, 1664 N. Virginia Street m/s 0274, Reno, NV 89557, United States of America.
Tel: +1 775-682-8347
Fax: +1 775-784-1340
Email: nicholasmurray@unr.edu
Handling editor:
Michal Heger
Department of Pharmaceutics, Utrecht University, the Netherlands
Department of Chemistry, Utrecht University, Utrecht, the Netherlands
Department of Pathology, Erasmus Medical Center, the Netherlands
Department of Pharmaceutics, Jiaxing University Medical College, Zhejiang, China

