-
Home
-
About JCTR
-
Gold Open Access
-
Issues
-
Editorial board
-
Author guidelines
-
Publication fees
-
Online first
-
Special issues
-
News
-
Publication ethics
-
Partners
-
Submit your manuscript
-
Submit your review report
-
Editorial Office
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. ISSN print: 2382-6533 ISSN online: 2424-810X
Volume 8 Issue 5
Aging increases the risk of flap necrosis in murine models: a systematic review
John P. Garcia, Francisco R. Avila, Ricardo A. Torres-Guzman, Karla C. Maita, Abdullah S. Eldaly, Luiza Palmieri, Omar Emam, Claudia C. Chini, Eduardo N. Chini, Antonio J. Forte*
Garcia et al. J Clin Transl Res 2022; 8(5):11
Published online: September 13, 2022
Abstract
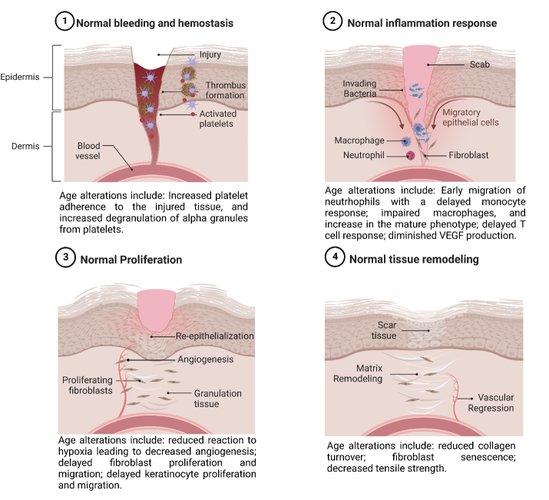
Background and aim: Although a natural phenomenon, aging is a degenerative condition that promotes cellular malfunction and subsequent organ and body dysfunction. According to the World Health Organization, the elderly are the fastest-growing age group worldwide. A 2012 population report stated that 43.1 million adults of 65 years or older lived in the United States, which is expected to jump to 83.7 million in 2050, placing an additional burden on an already stretched healthcare network. Elderly patients broadly impact our healthcare system, as reported in a 2014 wound report. 8.2 million patients were diagnosed with at least one type of wound, with patients 75 years or older making up most of the diagnoses. Aging affects all stages of the wound healing cascade. Although wound healing is downregulated in the elderly, scarce information exists regarding the effects of aging and flap survival in this group. Therefore, this study aims to report the impact of age on the survival of flaps in murine models. We hypothesize that increased aged animals will have decreased flap survival.
Methods: A systematic review was performed on February 1st, 2022, following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis. We searched for full-text articles written in English, consisting of experimental murine models that compared flap survival between aged and young animals, in the following databases: PubMed, Scopus, CINAHL, and Web of Science. The terms "mice" OR "rats" AND "surgical flaps" AND "aging" guided our search. Models affected by chronic diseases were excluded.
Results: Out of the 208 articles found by our search, seven were included according to our inclusion and exclusion criteria. Five studies used rats as experimental models, while the remaining two used mice. Local flaps were done in five studies, and two performed free flaps, transferring them from young and aged animals to young controls. Five articles reported lower flap survival in elder groups when exposed to ischemic insults. Three papers reported a deficiency in angiogenesis, vasculogenesis, and vascular reactivity as plausible causes for lack of survival, with one author correlating and verifying their results in human subjects. Although one article reported a lack of statistical power, they perceived a trend similar to the previous studies. Lastly, one article reported inconclusive and variable results.
Conclusion: Evidence suggests that a lack of angiogenic and vasculogenic response in conjunction with decreased vascular reactivity are responsible for the diminished survival of flaps in the elder. Therapeutic means to boost the angiogenic, vasculogenic, and vascular reactivity response to improve patient outcomes require further research to understand the time course and mechanisms of flap survival in the elderly.
Relevance for patients: All humans will feel the effects of aging one way or another. However, we can all agree that aging affects our basic biological processes, which negatively affects macroscopic appearance. One of the essential aspects downregulated in the elderly is their ability to respond to tissue injury and hypoxia, creating non-favorable circumstances for wound healing. Furthermore, to manage these non-healing wounds, flaps are raised to create a covering for these defects. However, age also impacts the ability of these flaps to survive, augmenting the problem and entering a vicious circle. To improve outcomes, we must focus our future research on understanding the basic principles of how aging affects the survival of flaps in the elderly population.
DOI: http://dx.doi.org/10.18053/jctres.08.202205.011
Author affiliation
1. Division of Plastic Surgery, Mayo Clinic, Jacksonville, Florida.
2. Department of Anesthesiology and Perioperative Medicine, Jacksonville, Florida.
3. Department of Basic Research, Jacksonville, Florida.
*Corresponding author
Antonio J. Forte
Division of Plastic Surgery, Mayo Clinic, 4500 San Pablo Rd, Jacksonville, FL 32224.
Phone: +1 904-953-2073
Fax: +1 904-953-7368
Email: ajvforte@yahoo.com.br
Handling editor:
Michal Heger
Department of Pharmaceutics, Utrecht University, the Netherlands
Department of Pharmaceutics, Jiaxing University Medical College, Zhejiang, China

