-
Home
-
About JCTR
-
Gold Open Access
-
Issues
-
Editorial board
-
Author guidelines
-
Publication fees
-
Online first
-
Special issues
-
News
-
Publication ethics
-
Partners
-
Submit your manuscript
-
Submit your review report
-
Editorial Office
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. ISSN print: 2382-6533 ISSN online: 2424-810X
Volume 8 Issue 5
Placental pathology, neonatal birthweight and Apgar score in acute and distant SARS-CoV-2 infection
Marie C. Smithgall*, Elisabeth A. Murphy, Sophie Rand, Ashley Sukhu, Sunidhi Singh, Nina Schatz-Siemers, Cathleen Matrai, Jiangling Tu, Christine M. Salvatore, Malavika Prabhu, Sallie Permar, Laura E. Riley, Brian D. Robinson, Rebecca N. Baergen, Yawei J. Yang*
Smithgall et al. J Clin Transl Res 2022; 8(5):5
Published online: September 7, 2022
Abstract
Background: Most research on SARS-CoV-2 infection during pregnancy has been on acute infections with limited data on the effect of distant infection.
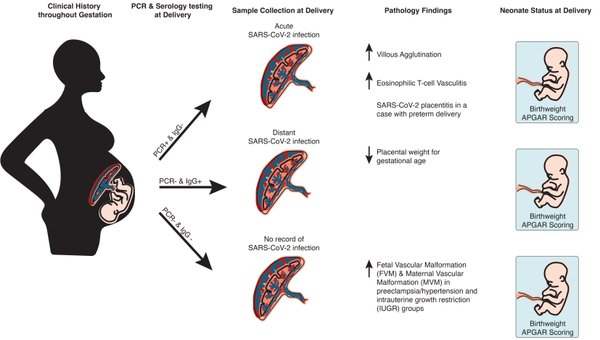
Aim: We examined placental pathology and neonatal outcomes in distant SARS-CoV-2 infection earlier in pregnancy compared to acute infections late in pregnancy/at birth and to non-SARS-CoV-2 infected patients with other placental pathologies/clinical presentations.
Methods: Placentas birthed to unvaccinated patients with SARS-CoV-2 RT-PCR testing and serology testing results from time of delivery were included in this study. A total of 514 singleton placentas between 4/18/2020 and 7/26/2021 were included: 77 acute SARS-CoV-2 infection (RT-PCR positive and serology negative); 222 distant SARS-CoV-2 infection (RT-PCR negative but serology IgG-positive); and 215 non-SARS-Cov-2 infected (RT-PCR negative, serology negative, and history negative) with other placental pathologies: preeclampsia/hypertension, intrauterine growth restriction (IUGR), diabetes, chorioamnionitis and meconium. Placental pathology findings, Apgar scores, and neonatal birth weights were compared.
Results: Placentas from the acute group had significantly more villous agglutination (10.4%, p=0.015) and eosinophilic T-cell vasculitis (5.2%, p=0.004) compared to placentas from the distant group (2.7% and 0%) and non-SARS-CoV-2 placentas (1.9% and 0.9%). One acute case showed SARS-CoV-2 placentitis and resulted in preterm delivery at 25 weeks. Both the preeclampsia/hypertension and the IUGR groups showed significantly more maternal vascular malperfusion findings compared to the acute (6.5%, 6.5% and 1.3%) and distant (7.7%, 7.7%, 3.2%) groups. Fetal vascular malperfusion findings such as thrombosis of fetal vessels (17.4% p=0.042) and intramural fibrin deposition (21.7% p=0.026) were significantly higher in the IUGR group compared to acute (7.8%; 2.6%) and distant (3.6%; 8.1%) infection. Many neonates born to patients infected with SARS-CoV-2 had birthweights outside of 95% confidence range of observed birthweights. There was no association of Apgar scores with infection status or placental pathology.
Conclusion: Acute and distant SARS-CoV-2 infections present differing placental pathology.
Relevance for patients: SARS-CoV-2 infection during pregnancy has demonstrable effects on the placenta with potential significant impacts for maternal and fetal health. Prevention of maternal SARS-CoV-2 infection, primarily through vaccination, remains the best mitigation strategy to prevent sequelae of maternal SARS-CoV-2 infection.
DOI: http://dx.doi.org/10.18053/jctres.08.202205.005
Author affiliation
1. Department of Pathology and Laboratory Medicine, Weill Cornell Medicine, New York, NY 10065 USA
2. New York-Presbyterian Hospital, Weill Cornell Medicine, New York, NY 10065 USA
3. Department of Pediatrics, Weill Cornell Medicine, New York, NY 10065 USA
4. Department of Obstetrics and Gynecology, Weill Cornell Medicine, New York, NY 10065
5. Weill Cornell Medicine, New York, NY 10065 USA
*Corresponding authors
Marie C Smithgall
Department of Pathology & Laboratory Medicine, 1300 York Ave, F-701. New York, NY 10065, USA
Tel: +1 212 746 3971
Fax: +1 212 746 8192
Email: mcs7003@med.cornell.edu
Yawei J Yang
Department of Pathology & Laboratory Medicine, 1300 York Ave, F-701. New York, NY 10065, USA
Tel: +1 212 746 3971
Fax: +1 212 746 8192
Email: yang@med.cornell.edu
Handling editor:
Michal Heger
Department of Pharmaceutics, Utrecht University, the Netherlands
Department of Pharmaceutics, Jiaxing University Medical College, Zhejiang, China

