-
Home
-
About JCTR
-
Gold Open Access
-
Issues
-
Editorial board
-
Author guidelines
-
Publication fees
-
Online first
-
Special issues
-
News
-
Publication ethics
-
Partners
-
Submit your manuscript
-
Submit your review report
-
Editorial Office
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. ISSN print: 2382-6533 ISSN online: 2424-810X
Volume 8 Issue 3
Outcomes of surgical resection of super-giant (≥ 15cm) hepatocellular carcinoma: Volume does matter, if not the size
Jia Jia Wee*, Chin Li Tee, Sameer P Junnarkar, Jee Keem Low, Yen Pin Tan, Cheong Wei Huey, Vishal G Shelat
Wee, et al. J Clin Transl Res 2022; 8(3):7
Published online: May 25, 2022
Abstract
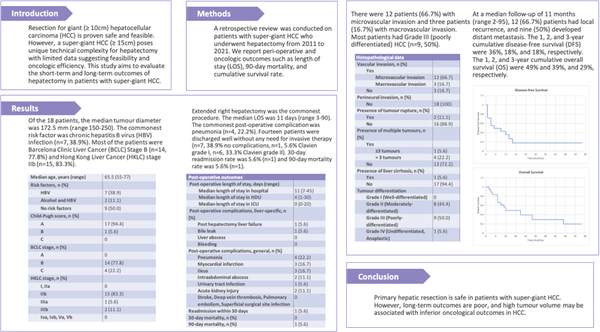
Background and aim: Resection for giant Hepatocellular carcinoma (HCC) (≥ 10cm) is deemed safe and feasible. However, a super-giant HCC (≥ 15cm) poses unique technical complexity for hepatectomy with limited data suggesting feasibility and oncologic efficiency. This study aims to evaluate the short-term and long-term outcomes of hepatectomy in patients with super-giant HCC.
Methods: A retrospective review was conducted on patients with super-giant HCC who underwent hepatectomy from 2011 to 2021. We report peri-operative and oncologic outcomes such as length of stay (LOS), 30-day readmission, 90-day mortality, and cumulative survival rate.
Results: Of the 18 patients, the median tumour diameter was 172.5 mm (range 150-250). The commonest risk factor was chronic hepatitis B virus (HBV) infection (n=7, 38.9%). Most of the patients were Barcelona Clinic Liver Cancer (BCLC) Stage B (n=14, 77.8%) and Hong Kong Liver Cancer (HKLC) stage IIb (n=15, 83.3%). Extended right hepatectomy was the commonest procedure. The median LOS was 11 days (range 3-90). The commonest post-operative complication was pneumonia (n=4, 22.2%). Fourteen patients were discharged well without any need for invasive therapy (n=7, 38.9% no complications, n=1, 5.6% Clavien grade I, n=6, 33.3% Clavien grade II). 30-day readmission rate was 5.6% (n=1) and 90-day mortality rate was 5.6% (n=1). There were 12 patients (66.7%) with microvascular invasion and three patients (16.7%) with macrovascular invasion. Most patients had Grade III (poorly differentiated) HCC (n=9, 50%). At a median follow-up of 11 months (range 2-95), 12 (66.7%) patients had local recurrence, and nine (50%) developed distant metastasis. The 1, 2, and 3-year cumulative disease-free survival (DFS) were 36%, 18%, and 18%, respectively. The 1, 2, and 3-year cumulative overall survival (OS) were 49% and 39%, and 29%, respectively.
Conclusion: Primary hepatic resection is safe in patients with super-giant HCC. However, long-term outcomes are poor, and high tumour volume may be associated with inferior oncological outcomes in HCC.
Relevance for patients: The presentation of super-giant HCCs may be asymptomatic and some patients are diagnosed late with limited treatment options. In some centers, this group of patients are denied surgical resection, and recommended for only locoregional therapies like TACE. This paper demonstrates that hepatic resection is safe and may be an option in patients who present at an advanced stage with a high tumour burden.
DOI: http://dx.doi.org/10.18053/jctres.08.202203.007
Author affilation
Division of Hepatopancreatobilliary Surgery, General Surgery, Tan Tock Seng Hospital, Singapore
*Corresponding author
Jia Jia Wee
Division of Hepatopancreatobilliary Surgery, General Surgery, Tan Tock Seng Hospital,
Singapore
Tel: +65 96255092
E-mail: jiajia.wee@mohh.com.sg
Handling editor:
Michal Heger
Department of Pharmaceutics, Utrecht University, the Netherlands
Department of Pharmaceutics, Jiaxing University Medical College, Zhejiang, China

