-
Home
-
About JCTR
-
Gold Open Access
-
Issues
-
Editorial board
-
Author guidelines
-
Publication fees
-
Online first
-
Special issues
-
News
-
Publication ethics
-
Partners
-
Submit your manuscript
-
Submit your review report
-
Editorial Office
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. ISSN print: 2382-6533 ISSN online: 2424-810X
Volume 8 Issue 3
Sarcopenia is the independent predictor of mortality in critically ill patients with cirrhosis
Saniya Khan#, Jaya Benjamin#*, Rakhi Maiwall, Harshita Tripathi, Puja Bhatia Kapoor, Varsha Shasthry, Vandana Saluja, Prashant Agrawal, Shalini Thapar, Guresh Kumar
Khan et al. J Clin Transl Res 2022; 8(3):6
Published online: May 25, 2022
Abstract
Background: Sarcopenia is strongly associated with poor outcome in cirrhosis. There is little prospective data that sarcopenia influences outcomes in critically ill cirrhotics (CICs). Computed tomography (CT) is the gold standard for sarcopenia assessment in the ICU, as it is independent of hydration status.
Aim: To assess the prevalence of sarcopenia and study its impact on clinical outcomes in CICs.
Methods: In this prospective observational study, CICs admitted to the liver ICU (LICU) were enrolled, if meeting inclusion (age 18-70 years, abdominal CT scan within three months prior to ICU admission) and exclusion criteria (survival likely to be <24 hours, coexisting chronic diseases). Clinical, hemodynamic, biochemical, nutritional parameters, including length of stay (LOS), duration of mechanical ventilation (MV), development of new-onset infections (NOI), incidence of new-onset AKI and overall survival were recorded. CT images at the L3 level were analyzed using Slice-O-Matic V4.3 software to assess the skeletal muscle index (SMI)- expressed as skeletal muscle area (cm2)/height (m2). Sarcopenia was defined if SMI was <50 cm2/m2- males and <39 cm2/m2- females. Data were analyzed using SPSS version 22.
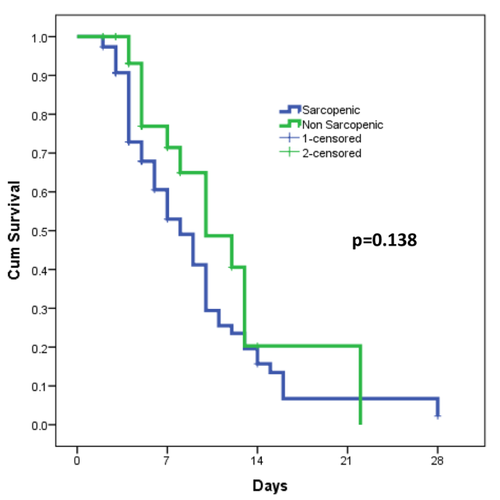
Results: Altogether 111 patients [M-83.8%; age 48.4±11.3 years; etiology: Alcohol- 56 (50.5%), NASH-27 (24.3%), Viral-12 (10.8%), Others-16 (14.4%); CTP-11.9±1.8; MELD-27.8±7.3; SOFA-10.5±4.1; APACHE-23±8; MV-54(48.6%)] were enrolled. Of these, 76 (68.5%) were sarcopenic and 35 (31.5%) non-sarcopenic. Sarcopenic CICs had higher overall mortality (72.4%) compared to non-sarcopenics (40%) [p=0.001, OR (95% CI)- 3.93 (1.69-9.12)], and higher prevalence of sepsis at ICU admission [53.9% vs. 31.4%, p=0.027, OR (95% CI)- 1.7 (1.0-2.92)] than non-sarcopenics. LOS, duration of MV, incidence of NOI, and development of new-onset AKI were comparable between groups. Multivariate binary logistic regression showed that sarcopenia, sepsis, and APACHE II score were independently associated with mortality.
Conclusion: Two-thirds of critically ill cirrhotics have sarcopenia at ICU admission, making them 1.7 times more susceptible to sepsis and increasing the risk of mortality by almost four-fold in the ICU.
Relevance for patients: Almost 70 % of patients with chronic liver disease admitted to the ICU have low muscle mass (sarcopenia). The presence of sarcopenia per se makes them highly prone to infections and increases the chances of death by almost four-fold; thus, highlighting the importance of nutrition optimization in this patient group.
DOI: http://dx.doi.org/10.18053/jctres.08.202203.006
Author affilation
1. Department of Clinical Nutrition, Institute of Liver and Biliary Sciences, New Delhi, India
2. Department of Hepatology, Institute of Liver and Biliary Sciences, New Delhi, India
3. Department of Anesthesia and Critical Care, Institute of Liver and Biliary Sciences, New Delhi, India
4. Department of Radiodiagnosis, Institute of Liver and Biliary Sciences, New Delhi, India
5. Department of Clinical Research, Institute of Liver and Biliary Sciences, New Delhi, India
#Contributed equally
*Corresponding author:
Jaya Benjamin
Department of Clinical Nutrition, Institute of Biliary Sciences, New Delhi, India
Tel: +91 9540951081
Email: jayabenjaminilbs@gmail.com
Handling editor:
Michal Heger
Department of Pharmaceutics, Utrecht University, the Netherlands
Department of Pharmaceutics, Jiaxing University Medical College, Zhejiang, China

