-
Home
-
About JCTR
-
Gold Open Access
-
Issues
-
Editorial board
-
Author guidelines
-
Publication fees
-
Online first
-
Special issues
-
News
-
Publication ethics
-
Partners
-
Submit your manuscript
-
Submit your review report
-
Editorial Office
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. ISSN print: 2382-6533 ISSN online: 2424-810X
Volume 7 Issue 6
Permanent pacemaker post-valve surgery: Do valve type and position matter? A propensity score matching study
Francesca Gatta*, Yama Haqzad, Mahmoud Loubani
Gatta et al. J Clin Transl Res 2021; 7(6):15
Published online: November 29, 2021
Abstract
Background and aim: This study evaluates whether aortic or mitral valve replacement with biological versus mechanical prostheses are independent risk factors for permanent pacemaker (PPM) post-cardiac surgery, alongside traditionally accepted determinants.
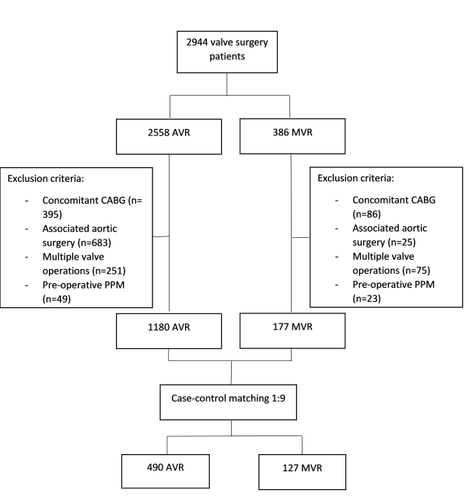
Methods: Single centre 10 years of retrospective activity. Case-control 1-to-9 matching (tolerance of 0.01) for 7 pre-operative and 2 intra-operative factors. Pearson Chi-Square test and one-way ANOVA for qualitative and quantitative analysis, respectively.
Results: After matching, 617 patients were included for analysis: aortic valve replacement, AVR (79.4% n=490) and mitral valve replacement, MVR (20.6% n=127). Permanent pacemaker was implanted in 3.7% (n=18) and 3.1% (n=4), p 0.8, respectively. A further analysis for PPM rate in biological vs mechanical prostheses did not provide any significant result (p 0.6 AVR and p 0.8 MVR). Post-operative complications in AVR and MVR groups were: re-opening (4.5% vs 6.3%, p 0.4), myocardial infarction (0.8% vs 3.2%, p 0.04), pulmonary (32.9% vs 38.6%, p 0.3), neurological (9.2% vs 11.8%, p 0.4), renal (9.8% vs 7.9%, p 0.5), wound (1.4% vs 2.4%, p 0.5), infective (5.5% vs 8.7%, p 0.2), multiple organ failure (4.9% vs 5.5%, p 0.6). The length of intensive care unit (hours) and hospital stay (days) was 71±163.8 vs 106.5±243.7 (p 0.5) and 14.7±14.7 vs 18.9±20.8 (p 0.01). In-hospital mortality resulted in 4.1% for AVR and 3.9% for MVR, p 0.9.
Conclusions: Valve position and valve type do not affect the likelihood of requiring permanent pacing in patients undergoing isolated aortic and mitral valve replacement.
Relevance for patients: A significant proportion of patients undergoing cardiac surgery develop arrhythmias and conduction disturbances post-operatively, often requiring the implantation of a PPM. Determining factors associated with an increase likelihood of permanent pacing would allow the optimisation of per- and intra-operative care, with the aim of reducing the incidence of patients requiring post-operative PPM insertion.
DOI: http://dx.doi.org/10.18053/jctres.07.202106.015
Author affiliation
1. Cambridge University Hospitals, Cambridge, UK
2. Hull University Hospitals NHS Trust, Hull, UK
*Corresponding author
Francesca Gatta
Cambridge University Hospitals, Cambridge, UK
Email: Francesca.gatta@addenbrookes.nhs.uk
Handling editor:
Michal Heger
Department of Pharmaceutics, Utrecht University, the Netherlands
Department of Pharmaceutics, Jiaxing University Medical College, Zhejiang, China

