-
Home
-
About JCTR
-
Gold Open Access
-
Issues
-
Editorial board
-
Author guidelines
-
Publication fees
-
Online first
-
Special issues
-
News
-
Publication ethics
-
Partners
-
Submit your manuscript
-
Submit your review report
-
Editorial Office
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. ISSN print: 2382-6533 ISSN online: 2424-810X
Volume 7 Issue 6
The concurrence of an enterocutaneous fistula and granulomatosis with polyangiitis: The role of immunosuppression as a bridge to definitive surgical treatment
Imad Hachem, Roy Hajjar, Frank Schwenter, Jean-Richard Goulet, Herawaty Sebajang*
Hachem et al. J Clin Transl Res 2021; 7(6):9
Published online: November 6, 2021
Abstract
Background and aim: Granulomatosis with polyangiitis (GPA) is a systemic disease that consists of vasculitis and granulomatous inflammation, and that usually affects the respiratory tract, the ear, nose and throat sphere and the kidneys. GPA may also cause skin manifestations that include ulcerations, nodules, or papules. An enterocutaneous fistula (ECF) is an abnormal tract that connects the skin surface to the gastrointestinal system.
Method: We report the first case of an ECF as a concurrent clinical manifestation during a new-onset GPA in a 68-year-old male patient.
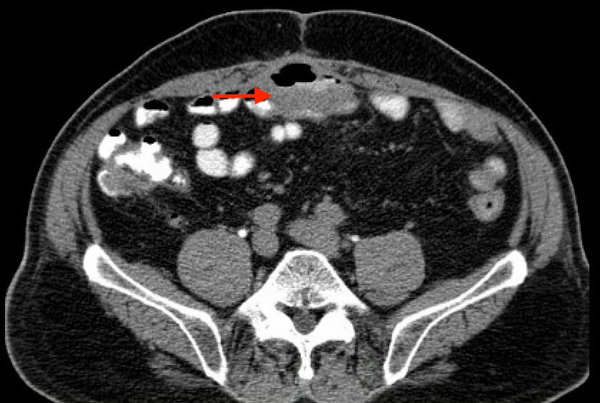
Results: The patient presented with an abdominal cutaneous wound with subcutaneous abscess, that evolved into an ECF with spontaneous enteric drainage. He also complained of nasal crusting, epistaxis, and cough, with further investigation revealing bilateral pulmonary nodules. Transthoracic biopsy was performed and was suggestive of necrotising vasculitis. A diagnosis of auto-immune vasculitis was highly suspected, and an immunosuppressive regimen of corticosteroid and intravenous cyclophosphamide was initiated. Significant improvement was noted in nasal manifestations, cough, and the output of the ECF. Definitive surgical management of the ECF was performed successfully.
Conclusion: To our knowledge, the presentation of a GPA with an ECF has not been previously reported, and poses major challenges to medical and surgical treatment, as it constitutes a dilemma as to how to address an auto-immune process requiring immunosuppression in the context of an infectious condition. This presentation suggests that immunosuppression in these patients may still be considered.
Relevance for patients: The concomitant presence of an ECF with abscess, an infectious process, and of an autoimmune disorder requiring immunosuppression is a major medical challenge. This case suggests that immunosuppression may still be considered in these patients to promote a better control of the concomitant ECF prior to definitive surgical therapy.
DOI: http://dx.doi.org/10.18053/jctres.07.202106.009
Author affiliation
1. Digestive surgery service, Centre hospitalier de l’Université de Montréal (CHUM)
2. Faculty of medicine, Université Laval
3. Department of surgery, Faculty of medicine, Université de Montréal
4. Department of medicine, Centre hospitalier de l’Université de Montréal (CHUM)
5. Department of medicine, Faculty of medicine, Université de Montréal
*Corresponding author
Herawaty Sebajang
Centre hospitalier de l’Université de Montréal, 1000, rue Saint-Denis, Montréal, Québec, Canada, H2X 0C1
Tel: +1 (514) 890 8000
Email: Herawaty.sebajang@umontreal.ca
Handling editor:
Michal Heger
Department of Pharmaceutics, Utrecht University, the Netherlands
Department of Pharmaceutics, Jiaxing University Medical College, Zhejiang, China

