-
Home
-
About JCTR
-
Gold Open Access
-
Issues
-
Editorial board
-
Author guidelines
-
Publication fees
-
Online first
-
Special issues
-
News
-
Publication ethics
-
Partners
-
Submit your manuscript
-
Submit your review report
-
Editorial Office
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. ISSN print: 2382-6533 ISSN online: 2424-810X
Volume 7 issue 3
Hospital length-of-stay among COVID-19 positive patients
Tze Chiam, Keshab Subedi*, David Chen, Eric Best, Federica B. Bianco, Gregory Dobler, Mia Papas
Chiam et al. J Clin Transl Res 2021; 7(3):10
Published online: June 5, 2021
Abstract
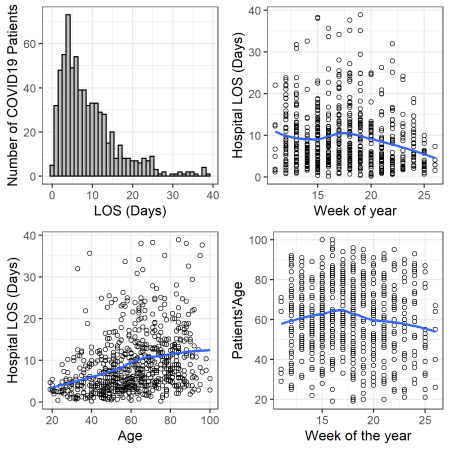
Background and aim: To determine COVID-19 patient demographics and comorbidities associated with their hospital length-of-stay (LOS).
Methods: Design: Single-site, retrospective study. Setting: A suburban 700-bed community hospital in Newark, Delaware, USA. Patients: Patients admitted to the hospital from March 11th, 2020 to August 11th, 2020 with a positive COVID-19 status. We followed a time-to-event analysis approach and used Kaplan-Meir curves and log rank tests for bivariate analyses, and an accelerated failure time (AFT) model for a multivariable model of hospital LOS.
Results: Six hundred and eighty-seven patients discharged alive (mean [SD] age, 60.94 [18.10] years; 339 men [49.34%]; 307 Black/African American [44.69%] and 267 White [38.86%]) were included in the investigation. Bivariate analysis using Kaplan-Meir curves showed that patients’ age, sex, ethnicity, insurance type, comorbidity of fluid and electrolyte disorder, hypertension, renal failure, diabetes, coagulopathy, congestive heart failure, peripheral vascular disease, neurological disorder, coronary artery disease and cardiac arrythmias to be significantly associated with LOS (p-values < 0.05). In the multivariable analysis, patients’ age, sex, ethnicity, number of Elixhauser comorbidities, and number of weeks since onset of the pandemic were significantly associated with LOS (p-values < 0.05). Fluid and electrolyte disorder is the only comorbidity independently associated with LOS after adjusting for patients’ age, sex, race, ethnicity, number of Elixhauser comorbidities, and weeks since onset of pandemic.
Conclusion: COVID-19 patients LOS varies based on multiple factors. Understanding these factors is crucial to improving the prediction accuracy of COVID-19 patient census in hospitals for resource planning and care delivery.
Relevance for patients: Understanding of the factors associated with LOS of the COVID-19 patients may help the care providers and the patients to better anticipate the LOS, optimize the resources and processes, and prevent protracted stays.
DOI: http://dx.doi.org/10.18053/jctres.07.202103.010
Author affiliation
1. Value Institute, ChristianaCare, Newark, Delaware
2. School of Public Affairs, Penn State University - Harrisburg, Middletown, Pennsylvania
3. Department of Physics and Astronomy, University of Delaware, Newark, Delaware
4. Biden School of Public Policy and Administration, University of Delaware, Newark, Delaware
*Corresponding author
Keshab Subedi
Value Institute, ChristianaCare, 4755 Ogletown-Stanton Rd, Newark, DE 19718
Tel: (701) 936-0792
Email: Keshab.Subedi@ChristianaCare.org
Handling editor:
Michal Heger
Department of Pharmaceutics, Utrecht University, the Netherlands
Department of Pharmaceutics, Jiaxing University Medical College, Zhejiang, China

