-
Home
-
About JCTR
-
Gold Open Access
-
Issues
-
Editorial board
-
Author guidelines
-
Publication fees
-
Online first
-
Special issues
-
News
-
Publication ethics
-
Partners
-
Submit your manuscript
-
Submit your review report
-
Editorial Office
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. ISSN print: 2382-6533 ISSN online: 2424-810X
Volume 7 issue 2
Is the use of dual antiplatelet therapy following urgent and emergency coronary artery bypass surgery associated with increased risk of cardiac tamponade?
Azar Hussain, Vassili Crispi, Shereen Ajab, Emmanuel Isaac, Ghazi Elshafie, Mahmoud Loubani
Hussain et al. J Clin Transl Res 2021; 7(2):3
Published online: March 13, 2021
Abstract
Background and aim: Cardiac tamponade is a recognised post-cardiac surgery complication, resulting in increased morbidity and mortality. The 2016 American College of Cardiology and American Heart Association Guidelines recommended the use of Dual Antiplatelet Therapy (DAPT) in the management of patients undergoing urgent or emergency coronary artery bypass grafting (CABG). The effect of DAPT on cardiac tamponade rates was investigated in comparison to aspirin monotherapy (AMT).
Materials and methods: Prospectively collected data from a tertiary cardiac surgery centre was analysed to identify the patients who underwent urgent and emergency CABG between January 2015 and January 2018. The patients were categorised as aspirin monotherapy (AMT) and Dual Antiplatelet Therapy (DAPT) groups. The primary outcome was total cardiac tamponade rate and secondary outcomes were length of hospitalisation and 30-days and 1-year mortality.
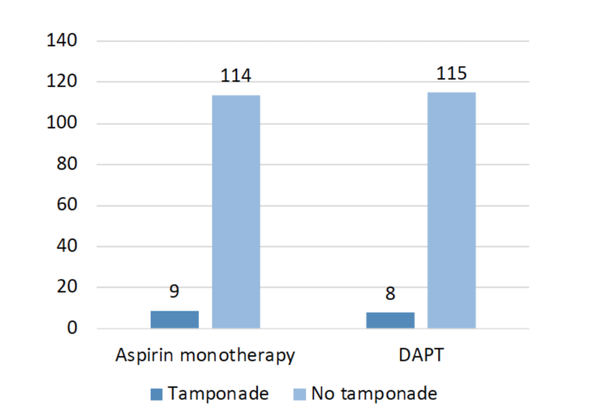
Results: A total of 246 eligible patients were included across both arms and compared for confounding variables. Cardiac tamponade was observed in 9 (7.3 %) and 8 (6.5 %) of AMT and DAPT groups respectively (p = 0.802). The average hospital stay in days was similar in both groups (AMT = 8.4 vs DAPT = 8.1, p = 0.82), whereas tamponade patients experienced a significantly longer hospitalisation when compared to non-tamponade patients (9.8 vs 8.1 days, p = 0.047). The 30-days and 1-year mortality was similar in both groups and were 0.8 % and 1.6 % respectively.
Conclusion: Overall, this study demonstrated that DAPT in urgent or emergency CABG patients is not associated with an increased risk of cardiac tamponade, length of hospital stay or mortality.
Relevance for patients: This study demonstrated that the use of DAPT in patients undergoing CABG as an urgent or emergency procedure following myocardial infarction is not associated with an increased risk of bleeding and has many associated benefits.
DOI: http://dx.doi.org/10.18053/jctres.07.202102.003
Author affiliation
1. Department of Cardiothoracic Surgery, Castle Hill Hospital, Hull University Teaching Hospitals NHS Trust, Hull, UK
2. Hull York Medical School, Allam Medical Building, University of Hull, Hull, UK
*Corresponding author
Azar Hussain
Department of Cardiothoracic Surgery, Castle Hill Hospital, Hull University Teaching Hospitals NHS Trust, Castle Road, Cottingham, HU16 5JQ, UK
Email: dr_azarhussain@hotmail.com
Handling editor:
Michal Heger
Department of Pharmaceutics, Utrecht University, the Netherlands
Department of Pharmaceutics, Jiaxing University Medical College, Zhejiang, China

